
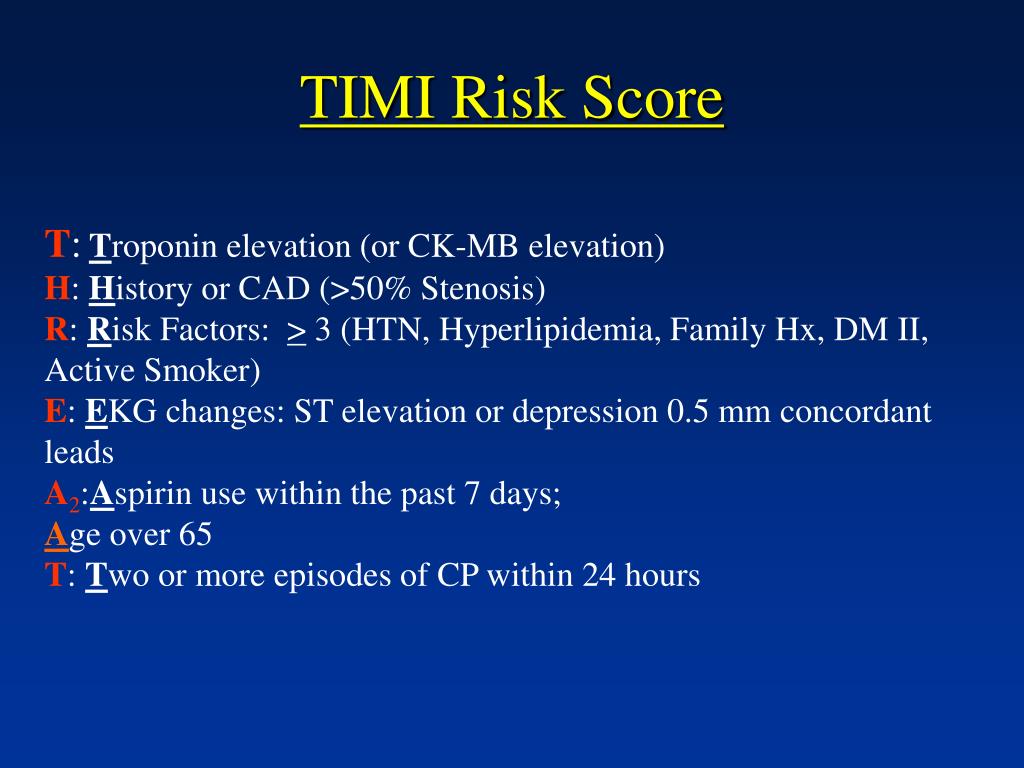
El objetivo es comprobar la eficacia del TRS en la estratificación del riesgo en una población con dolor torácico no seleccionada. Se ha demostrado que el TIMI Risk Score (TRS) es útil en pacientes con un riesgo intermedio y alto, pero faltan evidencias acerca de su aplicabilidad clínica en pacientes no seleccionados. Diferentes algoritmos de estratificación del síndrome coronario agudo (SCA) permiten identificar a los individuos con un mayor riesgo que pueden beneficiarse de tratamientos más agresivos. The score can identify high-risk patients who will benefit from hospital admission and early aggressive treatment. The TIMI risk score is useful for stratifying cardiovascular event risk in non-selected patients with chest pain. The relative risk of the composite endpoint per unit of TRS increase was 1.72 (95% CI, 1.32-2.24 P<.001). Of the patients who were initially admitted, 22 (6.4%) underwent revascularization, 4 (1.2%) had an MI, and 14 died (4.1%) from cardiovascular disease during follow-up. Patients with a high TRS had a significantly higher risk of reaching the composite endpoint of death, MI, or revascularization (relative risk per unit of TRS increase, 3.63 95% CI, 2.20-6.00 P<.001). Of the 911 discharged patients, 45 (5.3%) were admitted during follow-up: 9 (1.1%) underwent revascularization, 5 (0.6%) had a myocardial infarction (MI), and 2 (0.2%) died from cardiovascular disease. All cardiac events during 6-month follow-up were recorded. Overall, 343 (27%) were admitted and 911 (73%) were discharged. We evaluated 1254 consecutive patients (age, 54 years 57% male) attending an emergency department for chest pain. Our aim was to assess the efficacy of the TRS for risk stratification in a non-selected population with chest pain. However, little is known about its value in non-selected patients. The TIMI Risk Score (TRS) has been shown to be useful in intermediate- and high-risk patients. Stratification algorithms for acute coronary syndrome enable the identification of high-risk patients who will benefit from more aggressive treatment. Compared to other biomarkers, NT-proBNP is the strongest independent predictor of in-hospital and 180-day mortality.Introduction and objectives. In NSTE-ACS, NT-proBNP adds substantial information to the TIMI risk score and the ACC/AHA classification. NT-proBNP was not an independent predictor of risk of new myocardial infarction, even in the acute or long term. 001), and added significant prognostic information to the TIMI and ACC/AHA prognostic categories. Adjusting by clinical, ECG variables, and biomarkers, NT-proBNP concentration was the strongest independent predictor of in-hospital (OR 1.7, 95% CI: 1.31-2.20, p <. We prospectively studied the additive value of N-terminal probrain natriuretic peptide (NT-proBNP) in relation to the Thrombolysis in Myocardial Infarction (TIMI) risk score and the American College of Cardiology/American Heart Association (ACC/AHA) joint prognostic classification, and compared the predictive capacity of NT-proBNP, troponin T (TnT), C-reactive protein (hsCRP), myoglobin, and creatine kinase-MB (CK-MB) concentrations in a cohort of 1483 consecutive patients with non-ST-segment-elevation acute coronary syndromes (NSTE-ACS).Ĭentralised measurements of NT-proBNP, TnT, myoglobin, and hsCRP were performed 3 h (median) after admission.


 0 kommentar(er)
0 kommentar(er)
